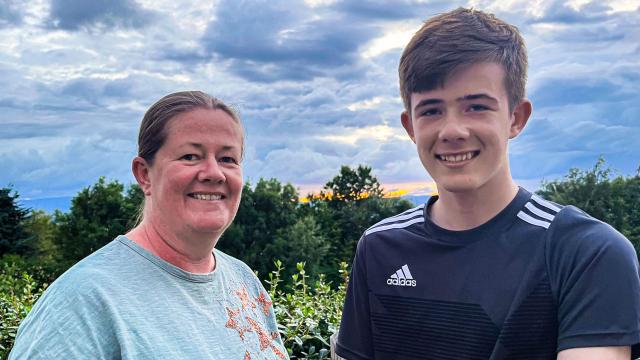
Hannah
"Diabetes Technology enabled me to focus on my studies and not have my diabetes completely occupy my mind. It gives reassurance and provides a comfort blanket for me."
Diagnosis
I was diagnosed with type 1 diabetes in March 2012, age 11. It was during my last year of primary school, as I was getting ready to transition to secondary school. My parents noticed that I was very thirsty and would grab a drink as soon as I got home from school. I’d also lost quite a bit of weight.
My parents weren’t that familiar with diabetes; however my Mum mentioned my symptoms to a friend who recognised that it could be diabetes. I then went to my local surgery where they tested my blood sugar which was very high and I was sent home to pack a bag and head to hospital.
Once I arrived at the hospital, I had a drip put in my arm which was quite a traumatic experience as they struggled to get it into a vein. The whole diagnosis was a lot to process as an 11-year-old and as a result of struggling with the drip, I developed a lot of anxiety around blood tests and hospital injections, which took me a few years to overcome.
The diagnosis was also a huge shock to myself and my parents and after being in hospital for a week and learning about blood sugar tests, injections & day-to-day management with the diabetes team, I returned home but couldn’t do the injections at first. So my Mum would have to come to school every day to give me my lunch-time injection, and I found it hard having 3 injections with food a day and a long-acting insulin injection in the evenings.
After a month or two following my diagnosis I was able to manage my injections independently. And around a year or so later I was able to go on my first insulin pump, so I wasn’t on injections for too long. I felt quite lucky at the time to have an insulin pump, although it was a relatively basic insulin pump just with two buttons to control it. However, I found it a lot more difficult to get access to a Libre and a CGM (Continuous Glucose Monitor), and we were self-funding my Libre until I qualified to get it on the NHS.
Access to Technology
As part of a research trial my first experience with CGM technology was while I was still with the Children’s Outpatients department at the hospital. I trialled a CGM that was only compatible with the pump I was on at the time, however I had a few problems with it and it didn’t work well for me, so I stopped using it. We then heard about Libre which I was really interested in, as I loved the idea of being able to see my blood sugar on my phone with just a scan instead of doing finger pricks. However, I was told it wasn’t available on the NHS unless you met certain criteria. At the time it felt like the people with poorer control got access to the best technology, which is understandable to improve their diabetes but frustrating for someone like me with pretty good control who couldn’t have an opportunity to experience the other benefits of this technology.
I was only able to get the Libre on the NHS after self-funding for around 6 months, which became very costly considering each sensor only lasts 15 days. While going through this process to have Libre funded on the NHS, I would always ask at every appointment if there was any update on CGM and if I would be able to apply for it. However, It was the same response that only people who met specific criteria could have it.
Going to University
In September 2019 I went to university to study Graphic Communication and moved into student halls in Birmingham. This was my first time living away from home and being on my own caused me to develop a lot of anxiety around night-time hypos. I felt like I had to set an alarm on my phone every night for around 2/3am so I could scan my Libre and check that my blood sugar was ok. So I was purposely waking myself up every night, and as a result I became consistently tired & I really struggled to focus on my studies.
After continually asking about having a Continuous Glucose Monitoring at my hospital appointments, my hypo anxiety & the impact on my sleep and day-to-day life studying became the springboard to enable me to apply for a CGM and prove that I really needed it. The CGM would automatically sound an alarm when my blood sugar goes high or low, and so I would only wake up when I actually needed to. This meant the CGM shifted from something I desired to improve my general quality of life with type 1 diabetes, to something that I needed to be able to properly look after myself and to focus on my university education.
Getting my Continuous Glucose Monitoring
The hospital wrote to the Clinical Commissioning Group (CCG) putting forward my case about my hypo anxiety and finally I was approved for a CGM. Unfortunately, we then had the pandemic which pushed things back further but I finally started on my CGM in March 2021, and it has honestly been life-changing! Particularly in my final year at university I was able to really focus on my work, knowing that the alarm would sound on my phone if my blood sugar went out of range. The intensity of the final year was a lot to deal with in itself, in weeks leading up to deadlines I would work on my projects from 9am-11pm most days, especially in the weeks prior to handing in my dissertation
My CGM enabled me to focus on my studies and not have my diabetes & blood sugar completely occupy my mind. As it should, my education and my university work became my main priority, and I don’t think I’d have been comfortable to do this had I not had the automation and constant monitoring of CGM. I have also been using Omnipod for over a year, and after many years of catching my insulin pump wire on the oven door, or drawer handles, a tubeless insulin pump made complete sense for me.
Following university, both CGM and my new insulin pump continue to greatly improve my quality of life. I’m now working as a full-time Graphic Designer for a private healthcare company, and the constant monitoring of CGM gives me reassurance and provides a comfort blanket for me. I have also recently started playing football a couple of times a week. I used to play prior to my diagnosis but navigating type 1 diabetes was difficult enough to deal with without the sport, so I stopped football not long after I was diagnosed. I now feel comfortable enough to return to it, knowing that the trend arrows on my CGM app enable me to essentially pre-empt a low and have food to avoid it. In adult life a continuous glucose monitoring is also massively helpful with driving, as again I can check it before I drive somewhere and if the trend arrows are heading down, I know to have something in order to avoid the low and prevent me from needing to pull over and pause my journey.
Equality with Technology
I feel passionately that there should be equal access and opportunity to diabetes technology. I feel there has always been an unfair system of needing to meet criteria to get access to CGM, when all people with type 1 diabetes should have the same technology options available to them. I would imagine there are a lot of people who haven’t had any exposure to diabetes technology and wouldn’t be aware of how much it could benefit them on a daily basis.
I found it very frustrating to have to push and fight for the opportunity to get funding on the NHS, in a system where people with Hba1c equates to priority access. While I can see how this makes sense with limited resources, its however unfair and arguably penalises people like me with good control. I think things are luckily starting to improve as charities like Diabetes UK highlight the need for more resources to be made available to people with diabetes, but I feel that more needs to be done and I hope that everyone will be able to experience the reassurance and benefits of Continuous Glucose Monitoring, as I have over the past 2 years.