If you have type 1 diabetes, your immune system has attacked the insulin-producing beta cells in your pancreas. This means you can’t make enough of your own insulin, and need to replace it through injections or a pump.
But insulin doesn't treat the underlying cause of type 1 diabetes: an immune system attack. This is what new treatments – called immunotherapies – will be able to do, by reprogramming the immune system so that it no longer destroys beta cells. In the future, they could stop type 1 diabetes in its tracks to delay, prevent or help to cure the condition.
The nuts and bolts of immunotherapy
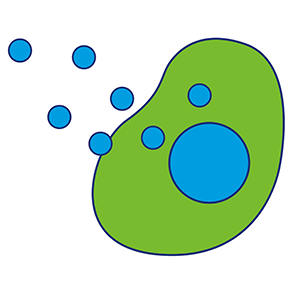
Our immune system is normally made up of a balance of different types of immune cells, all working together to protect us against infections. But in type 1 diabetes the immune system thinks insulin-producing beta cells are the enemy, and sets out to destroy them.
In type 1 diabetes there are different types of immune cells at work.
|
|
|
Different immunotherapies work in different ways, but they all aim to stop the immune system from attacking the pancreas. Some try to teach the B cells to no longer see beta cells as their enemy. Others try to dampen down the activity of B cells or killer T cells, so they can’t play their role. And some treatments help to boost the Treg police force so they can protect the pancreas against an attack.
Who could immunotherapies help?
Scientists believe immunotherapies could help people with type 1 diabetes at three time points.
Delay or prevent
Type 1 diabetes doesn’t develop overnight. Long before symptoms appear or a diagnosis is made, the immune system begins its attack. We can detect signs of this attack by testing for type 1 diabetes autoantibodies, to find people who haven't yet fully developed the condition, but are going to in their lifetime. Immunotherapies could be given to these people before too many of their beta cells have been destroyed, to hold off type 1 diabetes. Or, one day, prevent it entirely.
Stop
When people have just been diagnosed with type 1 diabetes the immune system hasn’t quite finished its attack and up to 20% someone's beta cells may still be alive. Immunotherapies could be used to preserve these beta cells. The more beta cells we can protect, the more insulin someone can produce on their own. This would make blood sugar management easier and protect against serious diabetes complications down the line.
Cure
Immunotherapies may also form part of a cure for people already living with type 1 diabetes for a longer time. Through our research and the Type 1 Diabetes Grand Challenge, we're supporting scientists to develop treatments to replace or regenerate beta cells that have been destroyed in type 1. Once we can do this, immunotherapies could be used alongside these cell therapies to protect new beta cells from further immune attack.
We're ambitious for a future where multiple immunotherapies are available to stop type 1 diabetes at its root in everyone at risk of, or living with, the condition. To get there sooner, we set up the UK Type 1 Diabetes Research Consortium, with an investment of £3 million and co-funding from Breakthrough T1D. It has brought scientists together and established a network of 30 specialist research sites across the UK to speed up the process of testing immunotherapies in clinical trials.
The next step is making sure those that are found to be safe and effective in trials are licensed for use in the UK, and can begin transforming lives as soon as possible. That's why we're working closer with the NHS to accelerate access.
