Eye damage caused by diabetes is called retinopathy. If left unchecked, it can lead to vision problems and eventually sight loss. But treatment options are currently limited, invasive, and don’t work for everyone. Research we’re funding right now is hoping to change this.
Blood vessels are mainly made up of two types of cells: endothelial cells that line the vessel wall, and pericytes that wrap around and support the endothelial cells. When retinopathy develops, the pericytes stop working properly and eventually die.
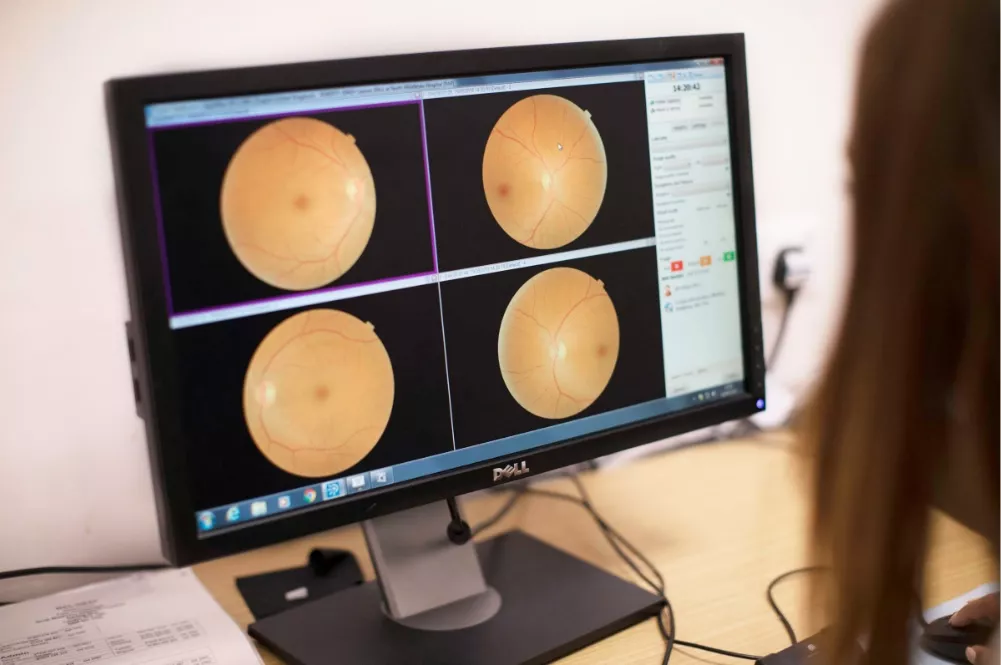
This causes blood vessels in the back of the eye, called the retina, to become leaky and damaged.
Our research in the 1980s pioneered the UK’s first eye screening programme for people living with diabetes, which continues to help us to spot early signs of retinopathy and intervene sooner.
While screening can identify this damage early on, current treatments are only effective once retinopathy has progressed to a later stage, meaning the condition can’t be treated until vision is affected.
So we critically need to understand more about how diabetic retinopathy is triggered, and to develop innovative new treatments that target it as soon as it’s detected.
Unlocking new treatments for retinopathy
Professors Stephen Moss and John Greenwood and their team at University College London have found that a protein in the retina, called LRG1, contributes to blood vessel damage that happens early on in retinopathy. With our funding, the team been working out the exact role LRG1 plays.
The team found that high blood sugar levels can cause high levels of LRG1, and having too much LRG1 is the first domino in the chain of events leading to the downfall of pericytes and blood vessels in the eye. By treating mice with diabetes with a new treatment that blocks the activity of LRG1, they were able to protect the mice’s eyes from retinopathy damage.
Revealing the impact of LRG1 gives us a better insight into how pericyte damage and sight loss can develop in people with diabetes. Professors Moss and Greenwood’s research is also a step towards testing new, anti-LRG1 treatments in people with retinopathy.
Ultimately, this could be life-changing for people with diabetes with early-stage retinopathy, or who current retinopathy treatments don’t work for.
Preventing damage to the retina
We also need a way to protect endothelial cells from the damage caused by high blood sugar levels. Activated Protein C (APC) is a protein that can protect and repair endothelial cells in other conditions, such as sepsis or stroke.
With our funding, Dr Judith Lechner and her team at Queen’s University Belfast have been testing how effective APC is at reducing the damage to endothelial cells in retinopathy.
They’ve been doing this by growing endothelial cells in the lab and exposing them to high levels of sugar, to mimic the damage seen in people living with diabetes.
So far the team have found that treating the lab-grown endothelial cells with APC can protect them, as it seems to strengthen the connections between the inside and outside of the cells. Next, the team plans to study these cells more closely to understand exactly how APC protects them.
Dr Lechner has also started testing APC in mice with diabetes. Traditionally, only male mice have been studied in diabetes research, as well as in many other medical fields. This is a problem when medications are studied in clinical trials in people, as there are potentially dangerous gaps in our knowledge of how treatments might affect women.
But Dr Lechner and her team have found a way to use female mice in their research as well. This means they can be more confident in their findings, and any future clinical trials of their treatment will be more reliable.
Dr Lechner’s research could help to develop new treatments to help slow the progression of retinopathy in its early stages, and protect people living with diabetes from this devastating complication. We’re looking forward to seeing what the team discovers next.
These two projects offer just a small glimpse into the research we’re funding to tackle retinopathy. Head to our research projects to find out more.
