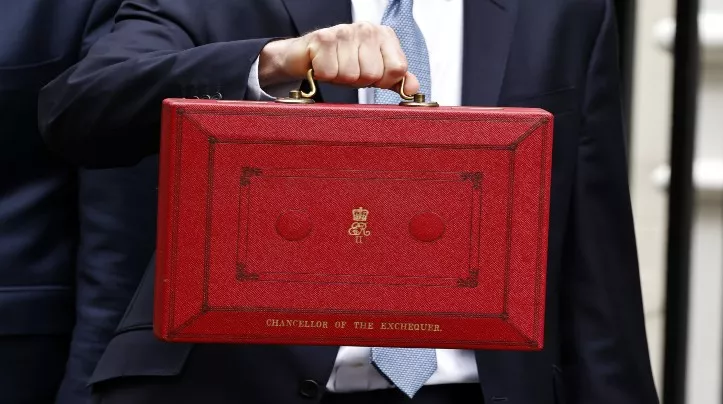
In January, we made a submission to HM Treasury setting out what we wanted to see from Chancellor Jeremy Hunt’s final Spring Statement before the next election to support people living with or affected by diabetes. But did it deliver?
Over five million people in the UK are now living with diabetes, equivalent to more than one in 14 people.
The majority of these are living with type 2 diabetes, with the number of people diagnosed with type 2 diabetes having almost doubled in the last 15 years. The number of people under 40 in the UK being diagnosed with type 2 diabetes is rising at a faster rate than the over-40s.
From January to March 2023, more than 360,000 working age adults living with diabetes were economically inactive because of long term sickness, a 43% increase from 2019. Of these, more than 40,000 listed diabetes as their main health condition for why they are not working, while 320,000 people listed diabetes as a secondary health condition.
Government measures have not gone far enough
This is the last Spring budget before the upcoming general election, and the government needed to make it count.
We saw welcome commitments on stopping smoking, but further measures to improve public health have not gone far enough to make sure government is using this time wisely to support people with and at risk of diabetes.
If people with diabetes do not get good routine care and support they find it harder to live well with diabetes and are more at risk of developing devastating and costly complications.
We know that people living in the poorest households are more than twice as likely to be living with type 2 diabetes than those with the highest household income. We are concerned that the tax cuts announced on Wednesday will benefit the poorest people the least.
In the Autumn Spring Statement 2023, we were also incredibly disappointed that the Chancellor announced planned changes to benefits. We expect these plans will have a profound impact on people living with diabetes in the future and make it even harder to stay healthy and remain in or return to work.
We know all too well from listening to people with diabetes who are impacted by health inequalities as part of Our Tackling Inequalities commission how difficult it can be to remain in suitable good-quality employment when you’re living with diabetes, or caring for someone who is.
What we wanted to see announced
We think the Spring Statement needed to focus on putting money in people’s pockets and funding the NHS and local authorities. It did not go far enough and we still want to see:
-
Action to tackle the cost of living for people impacted the most. As our report The Hidden Cost shows, we know the impact the cost of living is having on people with diabetes. We anticipate that the rising cost of living will lead to more people developing health problems, embedding poor health outcomes across the UK and widening existing inequalities. We are concerned that more people with diabetes will develop serious complications, and more people will be put at risk of developing type 2 diabetes.
-
Investment in primary and secondary prevention - so that people can avoid developing type 2 diabetes in the first place, and people living with diabetes can live well and free of complications.
-
Continued support to sustain successful NHS diabetes programmes - such as the NHS Diabetes Prevention Programme (DPP) and the NHS Diabetes Path to Remission Programmes in England.
-
Support for the newly diagnosed. We know how much it matters to get the right support when you’re first diagnosed with diabetes. This support makes a significant difference to quality of life, supports self-management and helps prevent complications and poor outcomes.
-
A public health funding uplift. Public health services are critical for improving the population’s health and reducing health inequalities. But local authorities need stable funding arrangements to carry out long-term planning and investment so they can tackle the root causes of worsening health trends and target programmes such as NHS Health Checks on those who are at highest risk of type 2 diabetes.
-
The potential and limitations of weight loss drugs are explored to make sure that the best health outcomes aren’t limited to people who can afford these privately, and acknowledging the impact on individuals, supply and cost mean they are only a small part of obesity prevention.
-
Fiscal measures to reduce obesity. It needs to be as easy and accessible as possible for everyone to have a healthy diet at no extra cost through reformulation and reduction of the consumption of unhealthy products.
What we want to see next
This means that we are recommending that the government should:
-
Implement existing commitments to reduce obesity, including delayed plans to protect children from junk food advertising on TV and online. It must also enact bold fiscal measures to enable healthier diets via reformulation and reduction of consumption of unhealthy products. New measures should consider inequalities in access to healthy food and seek to address them by making healthier options more affordable and accessible.
-
Deliver an increased, sustainable, long term funding settlement for local public health in England. As members of the Obesity Health Alliance, we support an increase of at least £1 billion more per year in the public health grant, with future yearly increases aligned to increases in the NHS budget.
-
Ensure that the £100 million funding announced in March 2021 for weight management services is restored and made into a long-term funding package. We support measures to ensure that weight management services operate under a fully resourced system that offers and delivers equitable access to appropriate, tailored and sustained weight management and support services to people living with overweight and obesity.
-
Reform healthcare by investing in earlier interventions, diabetes technology and routine primary care, in order to reduce demand for NHS future services. Research has shown that vital routine care and support for people living with diabetes plays an important role in preventing and delaying complications.
-
Implement the NHS Long-Term Workforce plan, taking into account the anticipated rise in the numbers and complexity of needs of people living with diabetes. Investment in a wide range of roles is essential to support primary and community care to deliver good diabetes care and ensure that all health care professionals have a basic level of diabetes education.
We support an Essentials Guarantee
To ensure that the pressures from rises in the cost of living do not lead to further demand on the health system through worse health outcomes for those living with diabetes, we are calling on the government to ensure social security is enough to avoid going without essentials like healthy food.
That’s why we support an Essentials Guarantee, which will prevent many from skipping meals, switching off essential appliances such as fridges, and being unable to pay essential bills.
We also want the government to guarantee people with diabetes have protection against disconnection from energy supplies, and to implement a guarantee for workers to have the right to paid time off to attend medical appointments.
